Case Managers & Arranging Incontinence Products When Leaving Hospitals in the UK

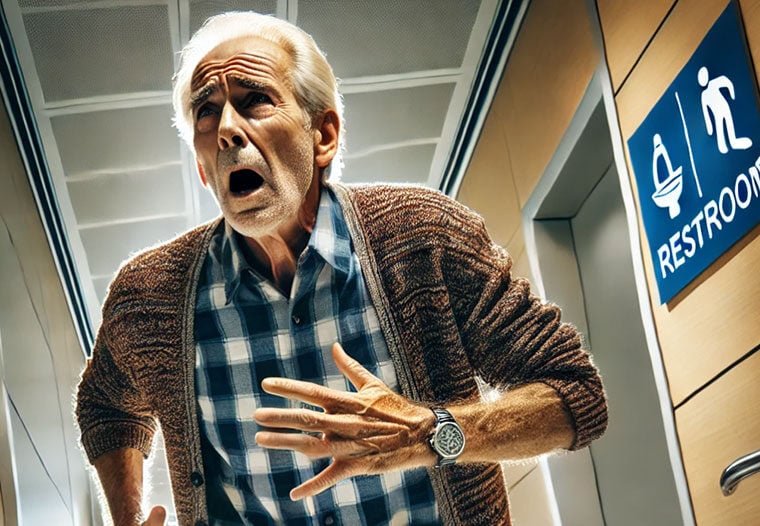
Male urinary incontinence is a deeply personal health issue that can be amplified during or after a hospital stay. In the UK, the discharge process for such patients includes a robust support system coordinated by the National Health Service (NHS), aiming to ensure continuity of care. Unlike in the USA, where access to incontinence products can hinge on insurance coverage, the UK model is need-based and centrally managed. Still, awareness of how to navigate the system is essential for caregivers of male patients, particularly older adults, to secure necessary continence support after discharge.
Introduction
While not every case of urinary incontinence is permanent, patients recovering from surgery, stroke, or those with frailty-associated incontinence often need support to manage symptoms at home. Case managers (also called discharge coordinators in the NHS) play a vital role in ensuring patients are not discharged without access to continence products, follow-up services, and proper caregiver guidance.
Understanding Male Urinary Incontinence
Urinary incontinence affects approximately 10–15% of men over the age of 65 in the UK. With an ageing population, this number is expected to rise. Causes vary and may include prostate enlargement, post-operative complications, neurological disease, or age-related decline in bladder control. Despite being common, many men underreport symptoms due to embarrassment, leading to delayed intervention and increased risk of skin issues, urinary tract infections, and loss of independence.
In the UK, GPs and community continence services work closely with hospitals to assess patients for suitable interventions, whether behavioral therapy, medical devices, or absorbent products. For hospitalized patients, early identification of incontinence risk during admission can trigger assessments and preparations for post-discharge needs.
Case Managers and NHS Discharge Planning
Discharge planning in the UK is primarily led by case managers who operate within NHS hospital teams. These professionals assess not just the patient’s immediate medical status but also their functional abilities and home environment. If a patient is likely to struggle with continence after discharge, this is flagged early on so that provisions can be made.
Unlike the fragmented private-public approach in the US, the UK has a more streamlined discharge protocol. NHS case managers collaborate with district nurses, social workers, and local continence advisory teams to ensure that upon leaving hospital, patients receive:
-
A continence assessment (either in-hospital or by community services post-discharge)
-
Referral to local continence services if needed
-
Short-term supply of incontinence pads or related products until a long-term plan is in place
In cases where patients lack informal caregivers or live alone, social services are also involved to arrange domiciliary care, including assistance with toileting and hygiene.
Arranging Incontinence Products Through the NHS
Access to incontinence products in the UK is usually via the local NHS continence service, not over-the-counter purchases. After discharge, the community continence team will assess the patient and determine what type of product is most appropriate—this might include absorbent pads, pull-up pants, or even male urinals or sheaths for more mobile individuals.
The key difference compared to the US is no payment is typically required. Products are delivered directly to the patient’s home at no cost, and there is no need for pre-authorisation or insurance negotiation. However, eligibility and quantity may vary slightly between regions, as local Clinical Commissioning Groups (CCGs) or Integrated Care Systems (ICSs) administer these services.
Patients may receive a basic quantity of pads monthly; if more are needed, they may have to supplement with self-funded options. Private suppliers exist in the UK, but these are typically only used when specific brands or extra stock is desired.

Caregiver Support and Responsibilities
In the UK, caregivers—often family members—play an increasingly critical role in managing male incontinence at home. Once a patient is discharged, the primary responsibility for their hygiene, continence management, and mobility support often shifts to the caregiver. The NHS acknowledges this by offering support in several forms:
-
Carer assessments through local authorities, identifying needs and providing equipment
-
Home visits by district nurses or continence advisors for training
-
Education on hygiene, skin care, and product use
Caregivers are taught how to apply and dispose of pads hygienically, monitor for pressure injuries or infections, and support the patient with toilet scheduling or bed transfers if mobility is compromised. Unlike in the US, where caregivers often struggle with the financial burden of medical supplies, UK caregivers benefit from a system where the basics are usually covered, provided the need is clinically justified.

Training and Education for Caregivers
While hospital stays may be brief, they serve as crucial windows for training. UK hospitals often schedule a pre-discharge meeting where nurses and discharge coordinators demonstrate proper use of continence products. This is particularly important for male patients who may be using new devices like sheath systems or urinals.
Further education is delivered through:
-
Leaflets or NHS website resources on managing incontinence
-
Follow-up visits from continence nurses
-
Support groups or helplines for carers of elderly men or those with dementia-related incontinence
For caregivers new to the role, this system offers reassurance that they are not alone and that help is available through local NHS services.
Follow-Up Care and Community Health Involvement
One of the UK’s strengths is its reliance on a community-based follow-up model. After hospital discharge, a community nurse or continence specialist often visits the patient’s home within days. This follow-up ensures:
-
Product supplies are adequate and suitable
-
No skin issues or complications are developing
-
Caregivers are coping with their responsibilities
If issues are identified, adjustments can be made, such as adding barrier creams or switching to different products. In contrast to the U.S. system, where patients may need to advocate for themselves within a commercial insurance structure, UK patients benefit from a model focused on needs assessment and clinical decision-making rather than cost.
Challenges in the UK System
Despite the strengths of the NHS system, there are some practical challenges:
-
Variability between regions: Some areas offer more generous product allocations than others.
-
Waiting times: Initial continence assessments may take several weeks in busy regions.
-
Limited product variety: NHS-supplied products may not suit everyone’s comfort or preference.
These limitations may push some patients or carers to purchase supplementary products privately. Fortunately, organisations such as Age UK, Bladder Health UK, and Continence Product Advisor offer guidance on what to buy and where.
Conclusion
In the UK, male patients with urinary incontinence benefit from a needs-based, centrally funded healthcare system where discharge planning, product supply, and caregiver support are all integrated within the NHS. Unlike the US model, there is minimal financial burden on the patient or caregiver, and decisions about product provision are clinically led.
Case managers and discharge coordinators ensure patients are not left to navigate this journey alone. With the backing of community services and free access to essential continence products, the UK model provides a strong framework for preserving dignity, reducing readmission risk, and improving quality of life after hospital discharge.
For male patients requiring innovative solutions to manage incontinence with dignity, QuickChange Wraps offer an effective and skin-friendly alternative. Now available in the UK, you can buy a 10 Count Trial Pack here or request a professional-use sample pack for healthcare institutions here.
References:
- NHS. (n.d.). Incontinence products. NHS. https://www.nhs.uk/conditions/urinary-incontinence/incontinence-products/
- NHS. (2023). Bladder and bowel nurse [Job advertisement]. NHS Jobs. https://www.jobs.nhs.uk/candidate/jobadvert/C9297-23-0332
- NHS England. (2018). Excellence in continence care: Practical guidance for commissioners, and leaders in health and social care. https://www.england.nhs.uk/wp-content/uploads/2018/07/excellence-in-continence-care.pdf
- NHS England. (n.d.). Plan for discharge. https://www.england.nhs.uk/urgent-emergency-care/improving-hospital-discharge/reducing-long-term-stays/plan-for-discharge/
- Royal Berkshire NHS Foundation Trust. (2025, February). Products for incontinence. https://www.royalberkshire.nhs.uk/media/znuhlt0r/products-for-incontinence_feb25.pdf

.jpg)