How to Prevent Moisture-Associated Skin Damage (MASD) During Incontinence
Patients who are bedridden or have limited mobility often experience skin damage. Such lesions become particularly severe if the patient's skin is not only exposed to pressure but also in prolonged contact with fluid or a moist surface. Even the smallest skin damage of this kind is extremely uncomfortable, not to mention severe conditions that require immediate intervention, treatment, and care.
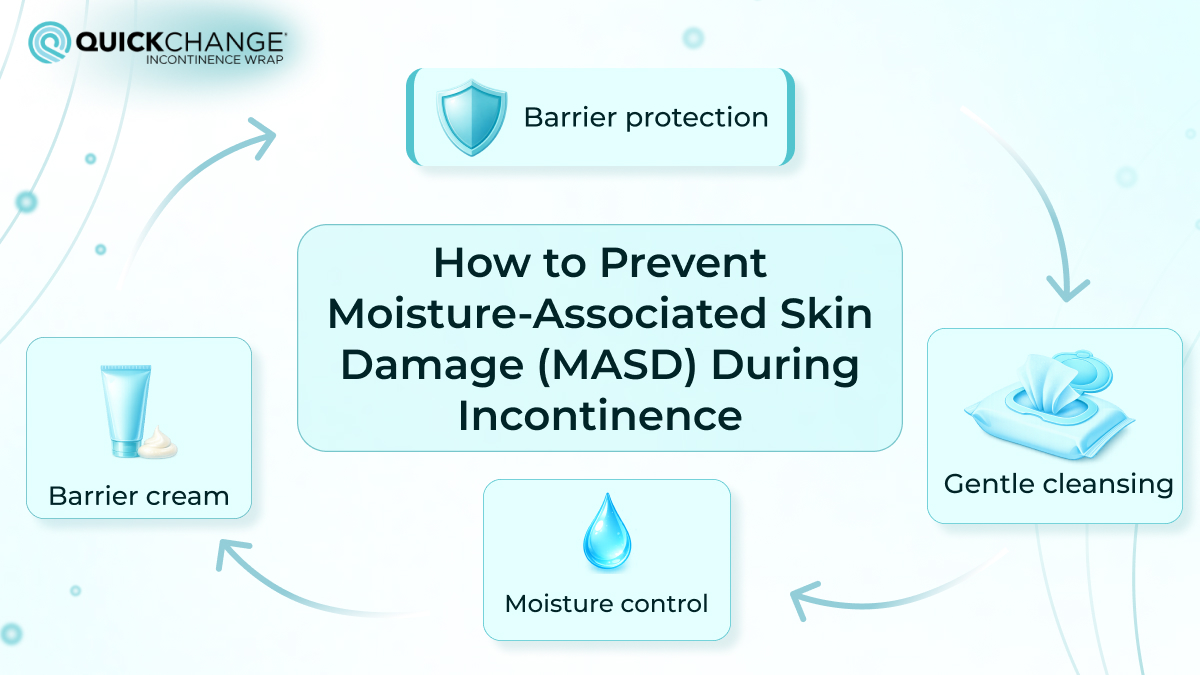
Moisture-associated skin damage (MASD) often affects patients with urinary incontinence. To avoid serious injuries, it is necessary to follow preventive care approaches, identify symptoms early, and choose high-quality incontinence products. We will discuss each of these aspects in detail in this article so that your patients or loved ones will not have to suffer from painful dermatological damage.
What is MASD Wound? Types and Causes
MASD is a medical abbreviation that refers to a general term for moisture-associated skin damage related to a group of inflammatory skin diseases caused by prolonged exposure to moisture, pressure, and irritants. In clinical practice, moisture-associated dermatitis most often affects men with urinary or mixed incontinence, when repeated contact with urine and/or feces gradually disrupts the integrity of the skin. MASD has four main forms:
- incontinence-associated dermatitis (IAD),
- intertriginous dermatitis (intertrigo),
- skin damage around a wound,
- skin damage around a stoma.
The key diagnostic feature is characteristic areas of skin damage that regularly come into contact with fluid. Such MASD wounds have a distinctive appearance, which can be seen in pictures of urine burns on skin. For effective prevention and treatment of wounds, it is essential to understand the structure of the skin. Read more about this further in the article.
Excoriation VS Maceration. Excoriated Skin Meaning
To better understand the topic of moisture-associated skin damage, which we will discuss in more detail below, it is necessary to clarify the excoriated skin meaning and how it differs from skin maceration, as these are fairly common terms closely related to the topics of urine-burning skin and MASD treatment. Therefore, let us provide detailed definitions and explanations of these terms and highlight the key differences in maceration vs excoriation.
Maceration Meaning
Maceration is a common process of softening or soaking tissues under the influence of liquid. It can be either a natural process, such as the usual swelling of the skin in water, especially on the tips of the fingers or feet, that can be seen on macerated skin pictures, or a deliberate action to achieve a specific result.

Examples can also be found in cosmetology, where the skin around the nails is soaked in a special bath before removing the cuticles, and in doctors who constantly wear rubber gloves and have wrinkled palms due to perspiration. In response to the question, “Is skin maceration dangerous?”, the answer is no. Softening the skin with liquid is not dangerous in itself, as we constantly encounter it in everyday life. However, the maceration process makes the skin more vulnerable, especially to mechanical actions such as friction or pressure, causing damage known as excoriation or abrasion.
Excoriation Meaning
Excoriation, better known as abrasion, is a breakdown of the skin's integrity resulting from mechanical damage to the skin, such as scratching or scraping. It is a superficial defect that often results from intense itching, such as scabies, eczema, and others, and can also occur as a result of psychological disorders, such as dermatillomania. The main types of damage that describe excoriation are: scratches, scraped areas, scabs, and in chronic cases, scars.
In cases of incontinence, the skin is often exposed to maceration, which weakens the protective barrier and, in constant contact with the bed and under the pressure of the body, leads to excoriation.
The Barriers Function of the Skin and Its Exposure to Moisture
It is essential to understand the primary components and layers of the skin to comprehend why and to what extent fluids such as urine affect it, causing MASD wounds. The skin consists of three main layers:
- The epidermis is the main barrier against chemical, physical, and microbial influences.
- The dermis, which provides skin elasticity, nourishment to the epidermis, and thermoregulation.
- The hypodermis (subcutaneous layer) is the deepest layer that connects the skin to muscles and bones.
As a protector, the epidermis plays the most important role, absorbing all impacts. Its outer layer prevents the penetration of irritants and pathogens. In the context of moisture dermatitis, even the slightest prolonged exposure to moisture overloads the barrier component of the epidermis. This makes the skin less thick, prone to maceration, and more vulnerable to friction, excoriation, inflammation, and actual destruction. The longer the contact with moisture, the stronger the impact and the deeper the wound.
Details of Moisture-Related Skin Breakdown Occurrence
Prolonged contact with excessive moisture, whether urine, feces, sweat, or exudate, softens the stratum corneum, causing maceration, which in turn reduces resistance to mechanical stress such as friction and shear.
Urine, which is alkaline, increases the pH (measure of acidity in a liquid) of the skin and disrupts its natural acidic environment, while fecal enzymes become more aggressive at higher pH levels, accelerating damage to the epidermis.
This is a more in-depth explanation of the process of dermatitis associated with urinary incontinence, which is one of the most common and clinically significant forms of MASD, often accompanied by more severe conditions such as secondary fungal or bacterial infections.
Increased Susceptibility to Incontinence Dermatitis in Older Adults
Aging causes a slowdown in organ function, and as we know, the skin is the largest organ in the human body, and its function also deteriorates with age. Typically, it becomes thinner, less elastic, and less firmly attached to the subcutaneous structures. In addition, skin sebum production decreases, and epidermal renewal and regeneration slow down. All these factors weaken the barrier function, making the skin more vulnerable to MASD.
When it comes to incontinence, older people are even more vulnerable to skin damage due to chronic diseases common with age. The most common among them are diabetes and limited mobility, which, combined with urinary incontinence and weakened skin barrier function, can lead to significant wounds. Under the above circumstances, moisture-associated dermatitis can occur as a result of even short-term or repeated exposure to moisture. As it progresses, dermatitis will lead to infections and unbearable pain, which will intensify if left untreated. As you can see, moisture-associated skin damage should not be ignored, and active skin protection should not be neglected, especially for the elderly.
Main Risk Factors for Moisture Wounds in People with Incontinence
Having discussed all the details above, we can summarize the main internal and external factors causing moisture-related skin damage in elderly people and patients.
- Age. With age, the skin becomes thinner, cell renewal slows down, the amount of sebum decreases, and the skin's protective barrier weakens, increasing vulnerability to moisture.
- Diabetes. In addition to the effect of diabetes on urination, causing polyuria (increased frequency of urination), impaired blood circulation, also caused by diabetes, further compromises skin integrity, immunity, and regeneration, which also increases the risk of infection.
- Limited mobility. This prolongs contact with urine or feces and exposes the skin to friction, pressure, and shear.
- Cognitive impairment. It reduces awareness of urine incontinence incidents, delaying cleaning and protection.
- Occlusive products. The use of occlusive products can retain moisture and heat, increasing maceration, while liquid feces accelerate damage to the epidermis due to enzyme activity and pH changes.
Each of these factors should not be underestimated in care because, individually, and even more so in combination, they significantly increase the risk of MASD and dermatitis associated with urinary incontinence, emphasizing the need for careful monitoring and active skin care.
Types of Moisture-Related Skin Damage
MASD is divided into four main types, each of which is associated with prolonged exposure to moisture and disruption of the skin barrier.
1. Incontinence-associated dermatitis (IAD): Contact dermatitis from urine or feces, most commonly occurring with fecal or mixed incontinence. The alkalinity of urine and enzymes in feces break down the skin, creating wounds and causing pain, discomfort, aversion, and psychological stress. Risk factors include the aforementioned frequent bowel movements or urination and incontinence, poor skin condition, limited mobility, cognitive impairment, and occlusive products. The severity of IAD is assessed using measures such as the GLOBIAD.

2. Intertriginous dermatitis (ITD) or intertrigo: ITD occurs when sweat is retained between skin folds (neck, hands, chest, buttocks, legs), causing mirror-like redness. Treatment focuses on keeping the folds clean, dry, and ventilated, avoiding the use of powders or gauze.
3 and 4. Peri-Wound and Peri-Stomal Damage: Both occur when secretions from a wound or stoma come into contact with the surrounding skin, leading to erythema, maceration, and inflammation. Treatment involves drainage of moisture, treatment of underlying causes, and the use of protective coatings or properly fitted appliances.
Moisture-Associated Skin Damage VS Pressure Ulcer: Difference
Pressure ulcers are not the same as moisture-related skin damage. Distinguishing between them is extremely important for proper care and treatment. They differ significantly in terms of the type of damage, causes, appearance, and location. The main differences between MASD and pressure ulcers are summarized in this table:
|
Feature |
MASD |
Pressure Ulcer |
|
Location |
Commonly in skin folds, the anal cleft, or areas exposed to urine/feces |
Over bony prominences such as heels, sacrum, and elbows |
|
Necrosis |
No necrosis present |
May present with black necrotic tissue |
|
Depth |
Superficial, partial-thickness loss |
Can range from superficial to deep tissue involvement |
|
Color |
Diffuse, irregular redness; may appear as “kissing ulcers” |
Non-blanchable redness or blue/purple in dark skin; clear wound edges |
|
Shape |
Irregular, diffuse spots |
Circular or regular-shaped wounds |
To determine the type of damage in your patient or loved one and distinguish between moisture-associated skin damage and pressure ulcers, follow these steps:
- Determine the exact location of the wound. MASD occurs in folds or near the anal fissure, and pressure sores occur above bony prominences.
- Identify the color. A pressure ulcer has a more characteristic red color and even dark coloration.
- Assess the depth. MASD affects the surface layer of the skin; pressure sores affect much deeper layers.
- Observe the shape, MASD is diffuse and uneven, and pressure wounds have a more distinct and uniform shape.
- Clarify the symptoms by asking the patient about their well-being, pain or discomfort, and their location and intensity.
Incontinence Care for MASD Treatment
Management of urinary incontinence is extremely important to reduce moisture exposure and prevent skin damage. Management and care of urinary incontinence begins with a thorough assessment, including urine analysis for infection, review of medications, and monitoring of urination frequency using frequency or volume charts.
In addition, patients with urinary or mixed incontinence will require special incontinence products such as diapers, briefs, pads, or catheters. The type of product depends on the patient's needs. Active people should consider catheters for fluid drainage in everyday life, while bedridden male patients or people with limited mobility will benefit from wraps, such as QuickChange wraps. When it comes to using incontinence products for moisture-associated skin damage, consider these basic solutions:
- Catheters can be used temporarily to drain moisture from damaged skin areas, but their continuous use is not recommended due to the risk of infection when in contact with wounds.
- Absorbent pads and fluid retention products are the best solution, but their use in cases of skin breakdown from moisture should be carefully monitored to ensure that the skin is not in prolonged contact with moisture after an incontinence accident. Wraps should also be selected based on their absorbency so that the skin can remain dry and have minimal contact with urine. In addition, the materials of the product should not cause the skin to sweat. We recommend trying a trial pack of QuickChange incontinence wraps, which are designed to meet all of the above requirements.
Skin care for patients with incontinence should be structured and follow the “Cleaning, Protection, and Restoration” protocol. To do this, the following products are required:
- pH-neutral, soap-free cleansers to clean the skin after each episode of incontinence and dry the affected area in the open air to avoid repeated friction with cleansers.
- Special non-perspiring protective barriers to create a protective layer between the skin and moisture.
Urine skin irritation treatment measures support the skin's natural barrier, maintaining its moisture and elasticity. Immediate attention to incontinence and constant skin care are crucial for preventing MASD, reducing discomfort, and maintaining the patient's quality of life.
Types of Skin Protection Products Against Moisture and Damage
Skin protection products are essential for preventing early or further damage to the skin associated with moisture. These products act as a barrier between the skin and irritants such as urine, feces, or wound exudate, helping to maintain skin integrity. The choice of an appropriate protective product depends on the area, the condition of the patient's skin, the wetness level, and the severity of the damage. Skin protection products that can be used both in hospitals and for prevention under a doctor's recommendation include:
Creams: oil-in-water or water-in-oil emulsions that are durable and provide long-lasting protection. Look for creams that contain ingredients such as petroleum jelly, zinc oxide, or dimethicone.
Ointments: oily, semi-solid products based on petroleum jelly, perfect for treating serious skin damage.
Pastes: thick mixtures of ointment-like substances and absorbent powders that stick well to wet skin, but can be harder to wash off.
Lotions: Light liquid suspensions suitable for areas with mild lesions, which require more frequent application.
Films: transparent polymer coatings that form a protective barrier but have no active ingredients themselves.
Elastomeric skin protectants: contain acrylate tetrapolymers, adhere well to moist surfaces, reduce pain, and do not require frequent application.
Risks Associated with Incontinence Products
Incorrect selection of incontinence products and poor skin care significantly increase the risk of moisture-related skin damage. In the United States, the treatment of urinary incontinence is often based on the long-term use of absorbent products. Like many medical devices, pads can cause side effects when used incorrectly. Common side effects of wearing incontinence pads include skin irritation, excessive moisture retention, and increased friction in sensitive areas.
Wearing incontinence pads 24/7, especially without frequent changes, restricts air circulation and holds urine on the skin. This prolonged exposure weakens the skin barrier and creates an environment in which inflammation and damage can occur from both urine on the skin and sweating. As a result, many people develop a rash from incontinence pads, especially if the pads are too absorbent, do not fit well, or are not designed for prolonged wear.
Summary
Moisture-associated skin damage (MASD) is a common and serious complication among patients with urinary incontinence. Older age, chronic diseases, limited mobility, and cognitive impairment increase vulnerability, emphasizing the need for active care.
Early intervention, patient awareness, and regular monitoring are key factors in preventing complications. As a safe option for incontinence management and moisture damage prevention, we recommend trying QuickChange Wraps, which are designed to provide reliable moisture control, reduce skin impact, and support overall care for men with urinary incontinence.
FAQ
Can urine cause skin irritation or burns?
Yes, urine can cause irritation, but not burns. Early prolonged contact with it will weaken the skin barrier and cause redness, followed by pain and a burning feeling. Although urine does not chemically burn tissue, many people describe the pain and burning sensation as similar to burns.
Why does my urine burn my skin?
Urine itself does not cause burning, but prolonged contact with the skin and friction can cause it. Urinary incontinence, prolonged use of pads, and fragile skin or existing moisture-related skin damage can cause painful skin burning from urine.
Is MASD the same as a pressure ulcer?
No, these are different types of damage. MASD refers to moisture-associated skin damage caused by urine or feces, while pressure ulcers develop as a result of prolonged pressure and impaired blood circulation and can cause much more severe wounds.
This content is for informational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your GP or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read or seen here.
.jpg)
