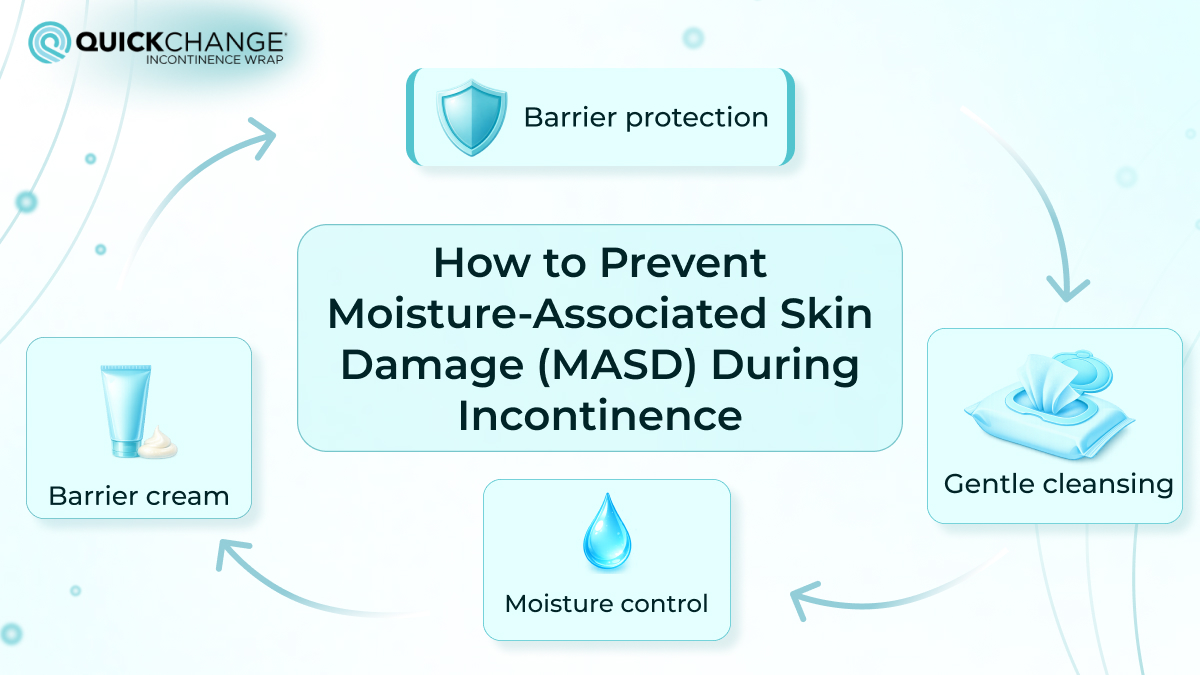
How to Prevent Moisture-Associated Skin Damage (MASD) During Incontinence
Patients who are bedridden or have limited mobility often experience skin damage. Such lesions become particularly severe if the patient's skin is not only exposed to pressure but also in prolonged contact with fluid or a moist surface. Even the smallest skin damage of this kind is extremely uncomfortable, not to mention severe conditions that require immediate intervention, treatment, and care.